- Section 1
-
Lesson 1
-
Last Lesson Experience
Empower
Course 3 of 5 in Provider Solutions
Genetic risk detection and managing hereditary cancer for patients
The Empower course is built to give healthcare providers, clinic staff, genetic counselors, and partners a deep, practical, and clinically relevant understanding of Natera’s Empower hereditary cancer test — what it is, when to order it, how to interpret the results, how to communicate with patients, and how to integrate it into practice workflows. We begin with foundations: why hereditary cancer matters, how inherited mutations increase lifetime cancer risk, what genes are involved, and why family history alone often misses people who carry high-risk variants. Empower screens for genes associated with increased risk for common hereditary cancers; the panels include multi-cancer options (40- or 81-gene panels) covering breast, ovarian, uterine, colorectal, pancreatic, melanoma, prostate, and other cancers. Natera+3Natera+3Natera+3
Next, this course covers use case scenarios: when a provider should consider recommending Empower — for patients with a strong personal or family history of cancer, early onset cancers, multiple primary tumors, or known mutations in the family; or in imaging/breast screening settings where genetic risk could alter screening frequency or modality. The ordering module includes patient selection criteria, sample/tissue requirements (blood or saliva), gestational or age limits if any, consent & counseling, and expectations around turnaround times. Natera+3Natera+3Natera+3
A major portion is devoted to interpreting results: what does a positive pathogenic or likely-pathogenic variant mean in terms of lifetime risk; how to use risk models (e.g. Tyrer-Cuzick for breast cancer + Empower results) to estimate risk; what action steps may follow (enhanced screening, risk-reducing surgery, lifestyle changes, medication); what does a negative result mean (but with residual risk based on family history / polygenic risk); how to deal with variants of uncertain significance (VUS), and how to determine if findings are extraneous (no immediate clinical action) versus those that deserve immediate feedback to the patient and possibly relatives. Natera+2Natera+2
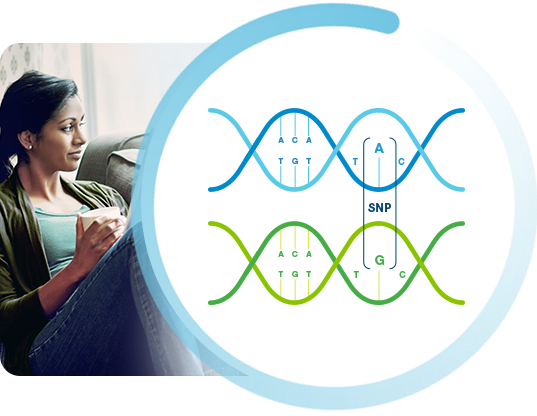
There is also a product background section: the science of hereditary cancer genes, how they are validated, how many genes are included in each panel, evidence basis, what published validation studies report in terms of sensitivity and specificity in diverse populations, coverage and limitations (e.g. what genes may have less evidence, what results may not change management, what patients might need follow-up). Natera+2Natera+2
Another module focuses on communication & patient discussion: how to order one of the Empower tests, then how to explain results clearly to patients — what increased risk means, what screening or preventive options exist, what options for family members are, how to address patient concerns such as anxiety, insurance or cost, how to explain what a VUS result means (often “not actionable at this time, but may need future reclassification”), how to help patients understand that negative result doesn’t eliminate all risk, especially if family history suggests risk.
The curriculum is comprehensive and structured, with video content, microlearning segments, downloadable resources (e.g. gene panels, Empower brochure, FAQ), interactive case studies (for example: a patient with early-onset breast cancer, a patient with Lynch syndrome family history, a patient negative on Empower but strong family history), quizzes, and tools for decision support.
Also included is guidance on workflow & implementation: how to embed Empower testing in oncology or high-risk clinics; how imaging centers or breast centers can integrate genetic risk assessment (family history intake, decision support tools), how to use the Natera Empower test requisition forms, how to ensure sample collection & shipping are smooth; how to manage result reporting and follow up; how to monitor patient outcomes.
An engagement strategy section shows how to drive uptake: how sales / provider outreach / clinical liaisons can connect providers to the course, how to use email campaigns, how to include links from the website / portals to training, how swimlanes can be set up (Get Started → Intro to Genetics → Empower Product Module → Ordering & Interpretation → Patient Discussion → Follow-Up & Screening Plan).
Finally, there is content on ethics, variant reclassification, familial cascade testing (identifying at-risk relatives), and how to support patient decision-making. Also, how to know when follow-up is required vs when findings are more informational, how to manage cost, insurance, and how providers can counsel patients in realistic terms.
By the end of this course, learners will be able to decide when to order Empower, understand the genes involved and the kind of risk increases associated, interpret results with nuance, distinguish urgent vs non-urgent findings, communicate results clearly and compassionately, counsel patients and families about screening/prevention options, understand limitations, integrate testing into their practice workflows, and engage their team and systems to ensure effective use of hereditary cancer testing in improving patient outcomes.
